Situation and Complication
The impact of record high inflation will begin hitting health plans in 2023, with costs estimated to rise on average by at least 6.5%. This will lead to higher insurance premiums and more costly care for both employers and employees. According to L.E.K. Consulting, some health systems are starting negotiations with requests for 30% rate increases. While prescription drug inflation is well anticipated, increases from Covid-impacted hospitals may surprise even the actuaries. Unfortunately, this comes at a time when many employers are trying to enhance benefits AND avoid cost-sharing increases – to boost employee recruiting and retention. Employers face the difficult task of managing rising costs and improving benefits without shifting the financial burden to inflation-weary employees.
Solution
Provide inflation protection for your health plan by validating the impact of your benefit solutions. Begin by scrutinizing the claim data to ensure vendors are performing and living up to their promised ROI. Then leverage these data-backed insights to make informed decisions to eliminate wasteful spending, reduce costs, and improve the quality of care. Actively managing your health plan to understand what’s working (and what’s not) will measurably improve the affordability of your benefit solutions.
Wellnecity Example
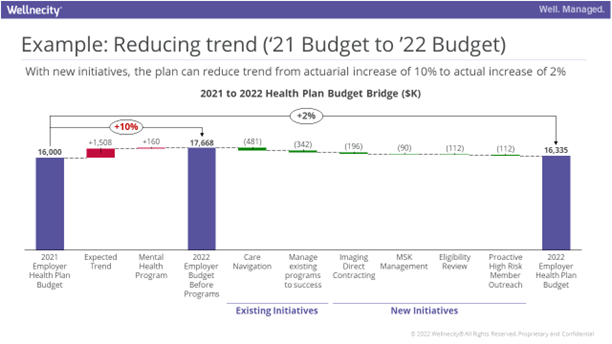
Self-insured employers and their Benefits Advisors have a small window to take steps to reduce spend before the full impact of inflation ripples through health care over the next several years. Understanding your health plan improvement options at the member level is the key to helping employees find quality care they can afford. In the example below, Wellnecity identified initiatives to mitigate trend to +2% rather than the anticipated actuarial trend of +10%, helping the employer manage spend to budget.