Situation
At the beginning of the COVID-19 pandemic, not just patients and providers were thrown into disarray. Health plan vendors and administrators were scrambling to define the impact of Covid on their health plan costs – current and future – namely which costs were Covid-related, e.g., diagnoses, treatment, medications, tests, and vaccinations, and which were not. Why did it matter? Two primary reasons: 1) Investors needed to understand the operating financials net of Covid health care costs and 2) Ability to capture planned government reimbursements.
Complication
For many self-insured employers, their TPA and PBM were unable to quickly report on these extraordinary expenses let alone adhere to evolving government guidelines. Without the ability to react, employers were unable to manage and unable to meet the needs of their investors or the federal government.
An alternative outcome
Due to our integrated health care claims data platform, Wellnecity was able to report on over 600 Covid-related cases and their related expenses – within weeks of the nationwide shutdown – before any other reporting was available.
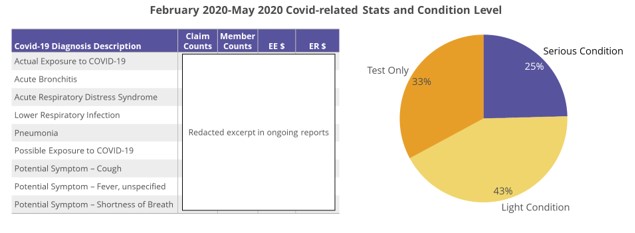
As Covid waves continued, Wellnecity has been able to identify and disaggregate Covid-related claims, track recoverable expenses, and monitor trends in both Covid-related and ordinary health plan expenses to forecast the future financial impact of this crisis.
Not only was Wellnecity able to inform real-time HR re-opening decisions, we enabled management to portray an accurate picture of Covid’s impact on healthcare cost (~$20M) on current and projected cost AND optimize requests for government compensation programs with detailed reporting.
