Situation
Stoploss reimbursements are critical to self-insured employers to mitigate the cost of catastrophic claims and to smooth out related financial shocks. Since 2012, the incidence of claims exceeding $1MM more than doubled — increasing about 10% each year.
Stoploss premiums are likely your health plan’s highest fixed cost. Despite this, employers must continue to pay increasingly high stoploss premiums (up 10% from prior year) to limit their claims liability and overall risk. Plan sponsors and brokers often bid stoploss annually in an attempt to lower this dreaded premium increase.
Complication
Stoploss policies are dense contracts, rife with actuarial language – and they get more complex as underwriters and plan sponsors negotiate over contracted liability. It’s convenient to trust that contracted terms are being administered correctly. In recent years, many employers are carving-out their stoploss to third-party standalone stoploss carriers due to their lower premium.
The reality is that due to this complexity, stoploss administration is often inaccurate.
Why?
- First, stoploss carriers are at the mercy of the claims data they receive. If they are a standalone stoploss carrier, they are dependent on the medical claims administrator (TPA/ASO) and the Pharmacy Benefit Manager to send them all eligible claims. When you have two vendors acting independently, claims aggregation errors often occur.
- Second, stoploss policies often include “run-out” claims that were incurred from a prior claims administrator. The prior carrier is not incentivized to send claims to stoploss for a terminated client. It is not unusual for 6-month (or indefinite!) data lags for these “run-out” claims.
- Finally, the seasonal increase in claims at year-end overwhelms claims administrators and stoploss eligible claims incurred at year-end are often not processed in time to meet the stoploss reimbursement terms. Watchful plan sponsors can find missed reimbursement opportunities that were incurred and received by the TPA/ASO but were not paid until the next calendar year, when the stoploss deductible has been reset to zero.
Solution
The best way to manage stoploss is to react quickly – by having current data that is aggregated across all vendors.
Top strategies for managing stoploss include:
- Active front-end bidding and claims forecasting based on historical claims data for your healthplan, not industry averages
- Accurate data on implemented clinical programs that contribute to avoided costs. This can enable negotiation with stoploss carriers before they increase your premium 10% again
- Manage stoploss reimbursements as actively as the front-end bid process
- Vendor management of all involved parties
Wellnecity Example
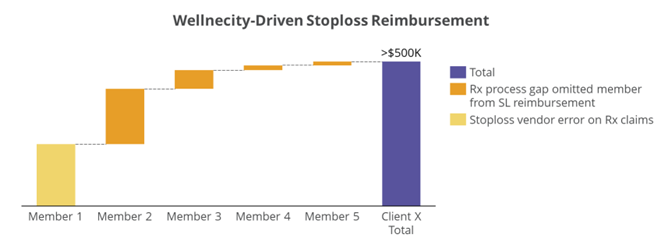
For one client, we detected a claimant who far surpassed the stoploss deductible but did not result in the employer receiving any reimbursements. The root cause was high-dollar pharmacy claims pushing the member over the threshold. The stoploss vendor failed to capture this case, not having both Medical and Rx claims aggregated properly.
Working with the employer and the stoploss vendor, Wellnecity provided accurately aggregated claims data that led to over $500K (~33% of their annual stoploss premium cost!) in additional reimbursement.
This was not a one-off scenario. Across , Wellnecity put ~$1MM back into the pockets of plan sponsors via active stoploss management.
