Situation
Who doesn’t love a good discount? There’s a reason why rebates have been around for over a century! Just as with common consumer goods, the pharmacy benefit manager model with up to 30% rebates appeals to our sense of shopping savvy. Through RFP processes, companies and their benefit advisers chase better discounts – or as one client put it – “I want to make sure I get my fair share.” Around 6 months after drug purchases occur, the employer gets their money back in the form of a quarterly rebate check.
So, what’s not to love about the pharmacy benefit management model of “capturing and passing-on” a generous portion of the rebates?
Complication
Answer: Misrepresentation of the real net price.
Delayed rebate payments with rebate percentages based on classes of drugs (rather than individual drugs) and the ability to modify these drug classifications make pricing and associated guarantees difficult to verify. Employers don’t really know how much they spend in any given financial quarter, AND they are challenged to evaluate alternative sourcing strategies because costs are not apples to apples.
But wait – there is more to what makes rebates a poor salve to manage Rx, a major and fast-growing component of health plan cost.
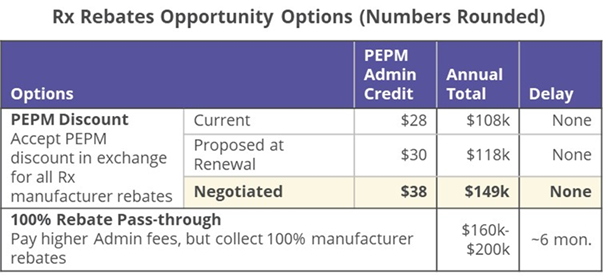
Instead of receiving rebates, some employers receive an admin credit instead of a rebate check. Good news the employer gets money sooner, bad news, they usually receive a lower percentage of the rebate, and worse news, the employer may be led to believe their admin costs are low (and do not need to be managed. That is, rebates effectively “reduce” the fixed costs of health plan management (network access, administration, broker fees, etc.). With this sleight-of-hand, rebates both reduce the cost of drugs AND fixed costs. In some cases, employers may be led to believe they have zero fixed cost!
Solution
The solution is to eliminate the distortion by gaining control over the data – creating a unit price that can be managed – by appropriately allocating the rebates to the relevant Rx expenditures.
While rebate rules are often restricted to protect PBM (Pharmacy Benefits Manager) – manufacturer contract terms, we know a lot about rebate terms (that’s why we ingest contract terms) and the distribution by drug class to create a highly accurate dataset with drug cost by member pre- and post- rebate.
With this information we can:
- Evaluate rebate performance
- Evaluate performance vs. contract guarantees
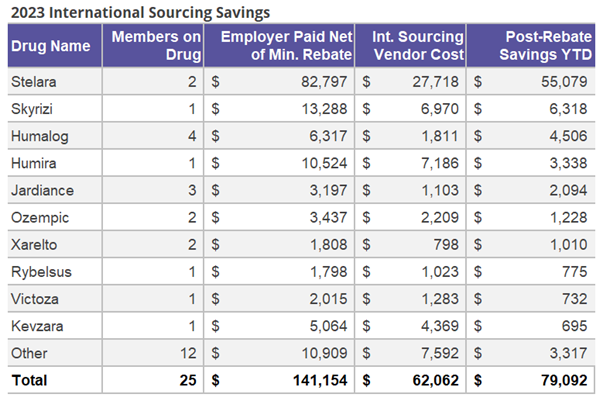
- Evaluate alternative sourcing solutions against post-rebate unit costs
- Accrue rebates in the period they were earned
- Understand current period financial performance
Or said differently – proactively manage health plan performance!
Wellnecity Example
For one client, we detected a claimant who far surpassed the stoploss deductible but did not result in the employer receiving any reimbursements. The root cause was high-dollar pharmacy claims pushing the member over the threshold. The stoploss vendor failed to capture this case, not having both Medical and Rx claims aggregated properly.
Working with the employer and the stoploss vendor, Wellnecity provided accurately aggregated claims data that led to over $500K (~33% of their annual stoploss premium cost!) in additional reimbursement.
In this example, we showed that the admin offset offered by the health plan was substantially below normal rebate ranges, enabling the benefit adviser to effectively negotiate for a substantially larger credit.