Situation and Complication
Care navigation is fantastic in concept. Employees generally lack clinical training and therefore don’t know how to properly navigate the health system, e.g., when to go to urgent care versus the emergency department, whether a procedure is necessary, and which provider will do the best job. Helping employees make informed choices leads to better care, lower cost, and fewer missed work days.
Unfortunately, expensive care navigation services often don’t work anywhere near as well as advertised. Why? Employees forget they have the service, aren’t inclined to call the insurance company for clinical guidance, don’t respond well to scripted call-centers, are distracted by their benefit questions, etc. At the same time, care navigators are often so inundated with benefit-related calls and transactional questions that they have little, if any, time to perform impactful, proactive outreach and give members in need helpful clinical guidance. The problem – employers don’t have the information to evaluate whether their care management programs are working, what the ROI is (based on claims data, not actuarial studies), and what they can do to improve performance.
Solution
The solution – figure out whether the care intervention programs in place are actually working. Because employers have access to their claims data, they can assess which employees would have benefited from outreach, e.g., employees with recent hospitalizations, multiple emergency dept. visits, 3 or more chronic conditions, >$5K spend in the last month. These lists can be compared with the outreach reports provided by the care navigation vendor to see if the members in need received the support they needed. The employer can then work with the vendor to improve performance, augment the solution set, or move to a better solution altogether.
Wellnecity Example
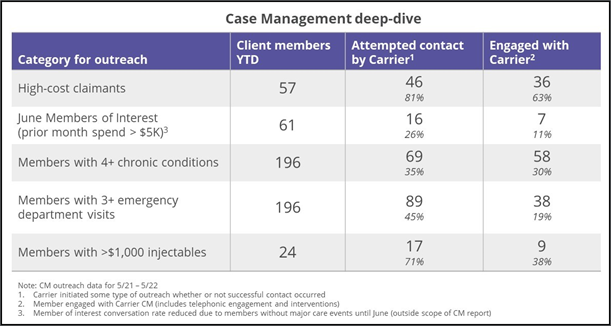
Unfortunately, measured performance is almost always disappointing. In Wellnecity’s experience, less than 1/3 of members needing support are receiving support, and even then, engagement levels are often lackluster. As mentioned above, navigators are swamped with inbound benefit-oriented calls, and generally not executing outreach to members in need. When navigators do outreach, the highest level of engagement is with high-cost claimants, i.e., members who are already well along in their care journey, by which point impact potential is limited.
The graphic below shows a standard comparison assessment (as referenced above) for best case situation. Notably, the high-cost claimants received the most engagement and the emerging cases and frequent emergency department visitors, the least.